CRM Features For USA HIPAA Compliance: A Comprehensive Guide
“CRM Features for USA HIPAA Compliance: A Comprehensive Guide
CRM Features for USA HIPAA Compliance: A Comprehensive Guide
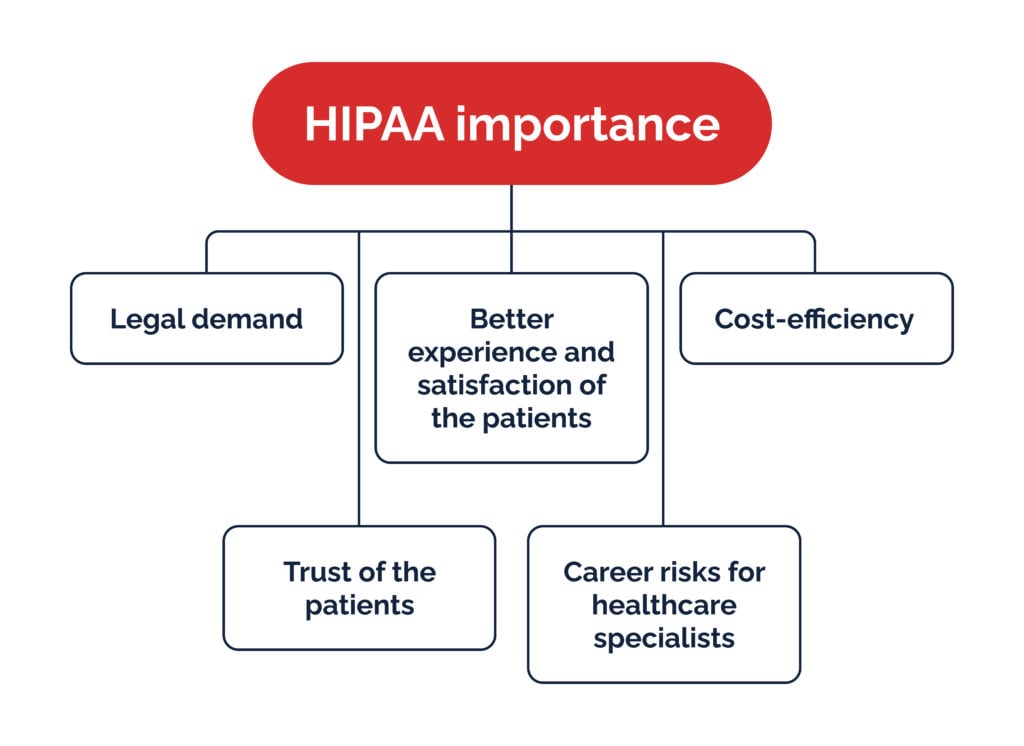
The Health Insurance Portability and Accountability Act of 1996 (HIPAA) is a US federal law designed to protect sensitive patient health information (PHI). For businesses handling Protected Health Information (PHI), particularly those using Customer Relationship Management (CRM) systems, compliance is not just a suggestion; it’s a legal necessity. Non-compliance can lead to significant financial penalties and reputational damage. This article explores crucial CRM features that ensure HIPAA compliance and help healthcare organizations maintain patient data security and privacy.
1. Data Encryption: The Cornerstone of HIPAA-Compliant CRMs
Data encryption is paramount for HIPAA compliance. At rest and in transit, PHI must be protected from unauthorized access. A HIPAA-compliant CRM should offer robust encryption methods, including:
-
Data Encryption at Rest: This protects data stored on servers and databases. Look for CRMs that use AES-256 encryption or stronger algorithms. This ensures that even if a data breach occurs, the encrypted data remains unreadable without the decryption key.
-
Data Encryption in Transit: This protects data transmitted over networks. A CRM should utilize HTTPS (secure HTTP) for all data transmissions, ensuring data is encrypted during transfer between the CRM system and users’ devices. This prevents eavesdropping and interception of sensitive patient information.
-
Key Management: Secure key management is critical. The CRM should employ strong key generation and protection mechanisms, preventing unauthorized access to decryption keys. Regular key rotation is also essential to mitigate the risk of compromise over time. Consider CRMs that offer features like hardware security modules (HSMs) for enhanced key management security.
Choosing a CRM with built-in encryption capabilities is far more secure than relying on third-party encryption tools, which can introduce vulnerabilities and complicate compliance efforts.
2. Access Control and User Authentication: Limiting Exposure to PHI
Restricting access to PHI is another crucial aspect of HIPAA compliance. A robust access control system is essential to ensure only authorized personnel can view, modify, or delete patient data. Key features to look for include:
-
Role-Based Access Control (RBAC): This assigns different levels of access based on user roles. For instance, a physician might have full access to a patient’s record, while a receptionist might only have access to basic contact information. This granular control minimizes the risk of unauthorized access.
-
Multi-Factor Authentication (MFA): MFA adds an extra layer of security by requiring users to provide multiple forms of authentication, such as a password and a one-time code from a mobile app. This significantly reduces the likelihood of unauthorized logins, even if passwords are compromised.
-
Audit Trails: A comprehensive audit trail logs all user activities related to PHI, including access, modifications, and deletions. This provides a valuable record for auditing and investigation purposes, helping to identify and address potential security breaches. These logs should be securely stored and protected themselves.
-
User Provisioning and Deprovisioning: The CRM should have a streamlined process for adding and removing users, ensuring that access is granted and revoked promptly as needed. This prevents former employees or contractors from retaining access to PHI.
3. Data Backup and Disaster Recovery: Protecting Against Data Loss
Data loss can have devastating consequences for healthcare organizations. A HIPAA-compliant CRM must include robust backup and disaster recovery mechanisms to protect PHI against various threats, including:
-
Regular Backups: Regular, automated backups of all PHI are crucial. These backups should be stored in a secure, offsite location to protect against data loss due to hardware failure, natural disasters, or other unforeseen events.
-
Disaster Recovery Plan: A comprehensive disaster recovery plan outlines procedures for restoring data and systems in the event of a disaster. This plan should be regularly tested to ensure its effectiveness.
-
Data Redundancy: Data redundancy ensures that multiple copies of PHI are available, minimizing the impact of data loss. This can involve replicating data across multiple servers or using cloud-based storage with data replication features.
The CRM vendor should be able to demonstrate their commitment to data protection by providing details about their backup and disaster recovery procedures.
4. Business Associate Agreements (BAAs): Establishing Legal Responsibilities
If your CRM provider handles PHI on your behalf, you must have a Business Associate Agreement (BAA) in place. A BAA is a legally binding contract that outlines the responsibilities of both parties regarding the protection of PHI. Key aspects of a BAA include:
-
Data Security Measures: The BAA should specify the security measures the CRM provider will implement to protect PHI.
-
Data Breach Notification: The BAA should outline procedures for notifying you in the event of a data breach.
-
Data Disposal: The BAA should specify how PHI will be disposed of at the end of the contract or when it is no longer needed.
Carefully review the BAA provided by your CRM vendor to ensure it adequately protects your organization’s interests and complies with HIPAA regulations. Don’t hesitate to negotiate terms to ensure your compliance needs are met.
5. Reporting and Monitoring: Maintaining Vigilance
Continuous monitoring is essential for maintaining HIPAA compliance. A HIPAA-compliant CRM should provide tools for:
-
Security Event Monitoring: Real-time monitoring of security events, such as login attempts, data access, and system changes, can help detect and respond to potential threats quickly.
-
Compliance Reporting: The CRM should provide reports that demonstrate compliance with HIPAA regulations. These reports should include information on access control, data encryption, and other relevant security measures.
-
Data Loss Prevention (DLP): Features that prevent sensitive data from leaving the system unauthorized. This might include tools to detect and block attempts to email or download PHI to unauthorized locations.
Proactive monitoring and regular reporting help identify vulnerabilities and ensure ongoing compliance.
6. Choosing the Right HIPAA-Compliant CRM: Due Diligence is Key
Selecting a HIPAA-compliant CRM requires careful consideration. Factors to consider include:
-
Vendor Reputation: Choose a reputable vendor with a proven track record of HIPAA compliance.
-
Security Certifications: Look for vendors with relevant security certifications, such as ISO 27001 or SOC 2.
-
Customer References: Check with other healthcare organizations that use the CRM to get their feedback on the vendor’s compliance efforts.
-
Contractual Agreements: Carefully review all contractual agreements to ensure they meet your organization’s needs and comply with HIPAA regulations.
Selecting a CRM is a significant investment, so thorough due diligence is essential to ensure you choose a solution that protects your organization from potential HIPAA violations and associated penalties. Don’t compromise on security; your patients’ data deserves the highest level of protection.
By implementing these features and exercising due diligence in choosing a CRM provider, healthcare organizations can significantly enhance their ability to comply with HIPAA regulations, safeguarding patient data and maintaining patient trust. Remember that HIPAA compliance is an ongoing process requiring continuous monitoring and adaptation to evolving threats.